|
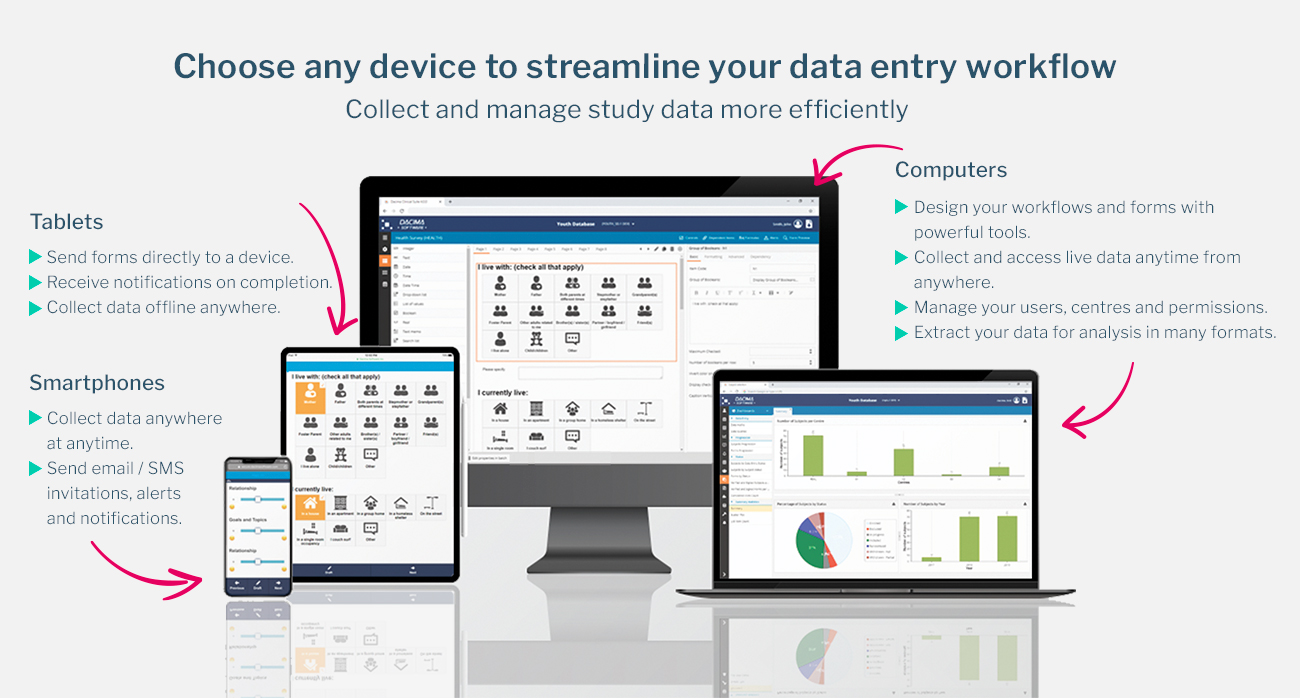
| data capture software |
Clinical trials today are more complex, global, and data-driven than ever before. As studies expand across multiple regions, involve diverse patient populations, and test increasingly sophisticated therapies, operational precision becomes essential. Among the most critical components ensuring trial integrity and efficiency are
Randomization and Trial Supply Managements, which together form the operational backbone of many modern clinical studies. When designed and executed correctly, these systems help protect scientific validity, improve patient safety, and reduce costly delays.
Understanding Randomization in Clinical Trials
Randomization is a core scientific principle used to reduce bias in clinical research. By assigning participants to treatment groups based on predefined probability rules rather than investigator choice, trials can ensure that differences in outcomes are attributable to the intervention itself rather than external factors.
Modern trials often use advanced randomization techniques such as block randomization, stratified randomization, or adaptive randomization. These approaches help balance treatment groups across key variables like age, disease severity, or study site. Effective randomization not only strengthens statistical credibility but also supports regulatory acceptance by demonstrating methodological rigor.
The Role of Trial Supply Management
While randomization governs how participants are assigned, trial supply management ensures that the right investigational products reach the right participants at the right time. This includes forecasting demand, managing inventory levels, tracking expiration dates, and coordinating shipments across trial sites.
Inadequate supply management can lead to serious consequences, including treatment interruptions, protocol deviations, and compromised data quality. Conversely, overproduction or poor forecasting can significantly increase trial costs. A structured approach to supply management is therefore essential to maintaining both efficiency and compliance throughout the study lifecycle.
Why Integration Matters
Historically, randomization and supply processes were often managed separately, leading to fragmented workflows and increased risk of errors. Today, integrated approaches to RTSM software allow these functions to work together seamlessly. When participant assignment is directly linked to supply allocation, trials can dynamically adjust inventory based on real-time enrollment and treatment needs.
This integration reduces manual intervention, minimizes the risk of unblinding, and supports consistent treatment delivery across sites. It also allows sponsors and research teams to respond quickly to changes, such as unexpected enrollment surges or supply chain disruptions.
Technology as an Enabler
Digital platforms have transformed how clinical trials are managed, particularly through the adoption of RTSM software. These systems combine randomization logic with supply chain controls into a single operational framework. By automating key processes, technology reduces reliance on spreadsheets, emails, and manual reconciliation.
RTSM software can provide centralized visibility into enrollment status, treatment assignments, and inventory levels across all sites. This visibility supports proactive decision-making, enabling teams to identify risks early and implement corrective actions before they impact the trial.
Supporting Blinding and Compliance
Blinding is a critical requirement in many clinical trials, particularly those designed to eliminate placebo effects or investigator bias. Integrated systems help maintain blinding by ensuring that treatment allocation information is restricted to authorized users only.
At the same time, regulatory compliance depends on accurate documentation and traceability. Automated systems generate audit trails that record every randomization event, shipment, and inventory change. This level of transparency is essential for inspections and helps demonstrate adherence to Good Clinical Practice (GCP) guidelines.
Managing Global and Decentralized Trials
As clinical research becomes increasingly global, operational challenges grow. Trials may span dozens of countries, each with unique regulatory requirements, import restrictions, and logistical constraints. Coordinating supplies across this landscape requires careful planning and continuous monitoring.
Centralized management tools make it easier to handle regional variations while maintaining consistent trial standards. By aligning randomization strategies with localized supply plans, teams can ensure uninterrupted treatment even in complex, decentralized trial models.
Reducing Risk and Improving Efficiency
Operational risk is an inherent part of clinical research, but it can be mitigated through thoughtful design and execution. Integrated Randomization and Trial Supply Management software help reduce risks related to misallocation, stockouts, and protocol deviations. Automation also decreases the likelihood of human error, which remains a leading cause of trial inefficiencies.
From a financial perspective, better forecasting and inventory control can significantly reduce waste. This is particularly important for studies involving high-cost investigational products or limited-supply therapies, where every unit must be carefully accounted for.
Enhancing the Participant Experience
Although these systems operate largely behind the scenes, they have a direct impact on trial participants. Reliable treatment availability ensures that participants receive their assigned therapy without delays or substitutions, which supports adherence and trust in the study process.
Efficient operations also reduce the administrative burden on site staff, allowing them to focus more on patient care and data quality. In this way, well-managed systems contribute to both scientific and human-centered outcomes.
Future Trends and Considerations
The future of clinical trial operations points toward even greater integration, real-time analytics, and adaptive design. Emerging technologies such as predictive modeling and artificial intelligence may further optimize supply forecasting and enrollment strategies.
As trials become more patient-centric and decentralized, systems will need to support home delivery, remote monitoring, and flexible treatment schedules. The principles underlying Randomization and Trial Supply Managements will remain essential, but their implementation will continue to evolve alongside scientific and technological advances.
Conclusion
In modern clinical research, operational excellence is inseparable from scientific success. Effective randomization ensures unbiased treatment allocation, while robust supply management guarantees continuity and compliance. When these functions are integrated through advanced systems and thoughtful planning, trials can achieve higher efficiency, lower risk, and better outcomes for all stakeholders.
By viewing these processes not as isolated tasks but as interconnected elements of a unified strategy, research teams can better navigate the complexities of today’s clinical trial environment and prepare for the challenges of tomorrow.